Digital PCR
The answers are in the sewage
n March 2020, one of Warish Ahmed’s colleagues saw a tweet from a University of Queensland researcher asking if anyone in Brisbane, Australia, could test for SARS-CoV-2 in raw sewage. Researchers in China had just announced they could detect the SARS-CoV-2 virus in the feces of infected people.
But what happened after the waste was flushed away to a wastewater treatment plant, where it mixed with the outflow from hundreds of thousands of toilets, sinks and drains? Were its genetic remnants still detectable? With testing methods for COVID-19 still being developed and distributed around the world, scientists were eager to find new ways to track cases to understand the scope of the pandemic.
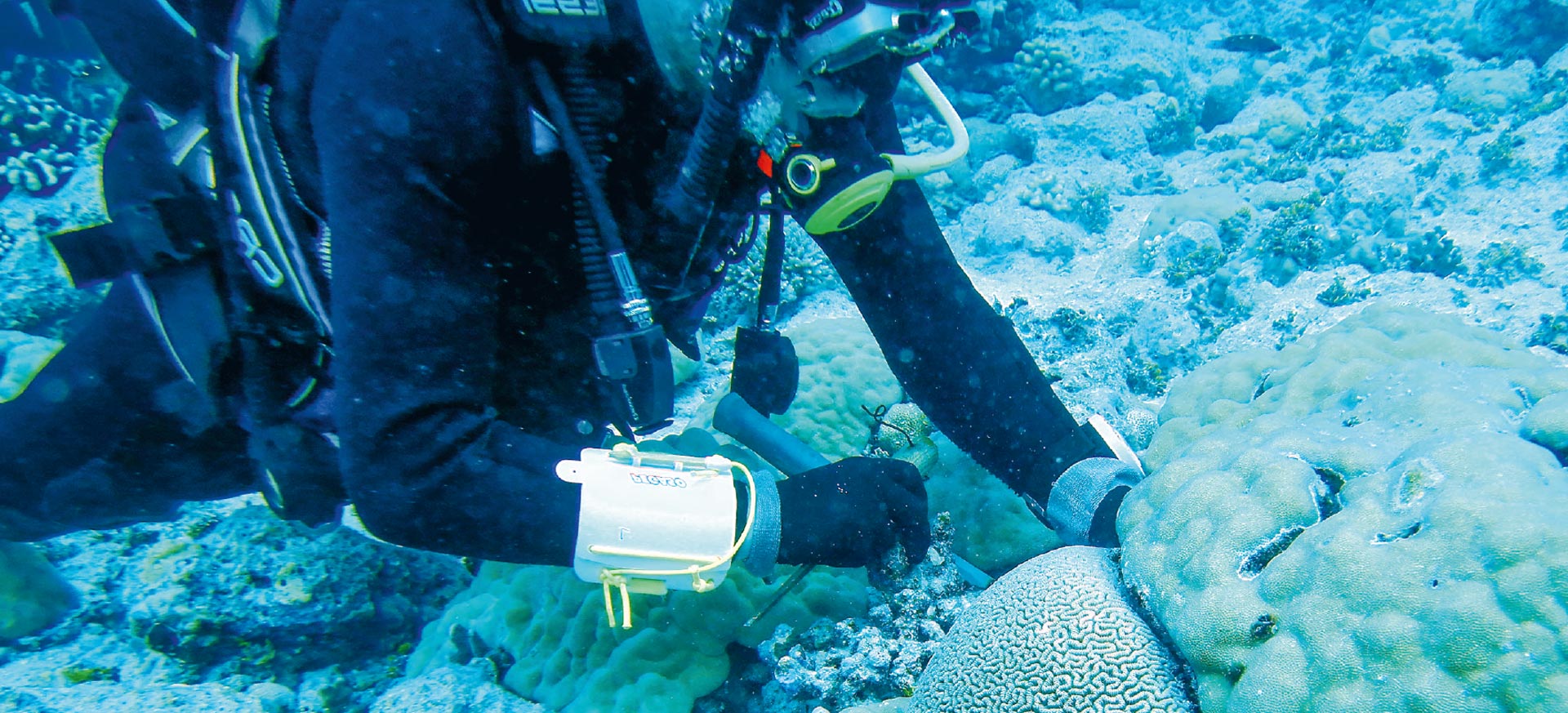
He immediately tagged Ahmed, a senior research scientist at the Commonwealth Scientific and Industrial Research Organization (CSIRO), Australia’s national science agency. Ahmed, whose lab specializes in microbial source tracking in water, otherwise known as MST, had long handled a variety of viral environmental samples from across Queensland. At the first reports of COVID-19 spreading outside of China, he had started work on an analytical method to detect SARS-CoV-2 RNA in wastewater, anticipating the value of an early detection system. The traces were bound to be minuscule when the number of cases was low, but he believed his highly sensitive molecular method could still detect them in raw sewage.
Ahmed tweeted that they should get in touch.
Later that afternoon, three researchers from the University of Queensland rang him. As part of routine drug monitoring, hourly samples were already being collected at treatment plants handling wastewater from Brisbane, Queensland’s capital. From these, they created 24-hour composite samples, each murky container representing hundreds of thousands of people. All they needed was the test.


is a senior research scientist in CSIRO Land & Water. He enjoys troubleshooting problems, implementing new ideas and putting them to the test. “I have studied science since my childhood,” he says. “I wanted to have a PhD in science, which was a very cool thing for a small-town boy from Barisal, Bangladesh.”
Pool-testing 600,000 people at once
The samples arrived at the CSIRO laboratory the next day. After first concentrating and then extracting the tiny amounts of RNA from the raw sewage, RT-qPCR tests found what they were looking for: faint but definite traces of SARS-CoV-2 RNA. Using a simple model, they roughly estimated that 171 to 1,090 people in the catchment area, which covers about 600,000 people, were potentially infected.
It was the first confirmed evidence of SARS-CoV-2 RNA in wastewater in Australia, and, says Ahmed, “the results were proof this method could potentially be used to identify hotspots and infected people.” They had struck upon what might prove to be a cost-effective way to pool-test entire communities for the disease.
When Ahmed and his colleagues published their proof-of-concept research, it created ripples in the scientific community.


partitions per well of a digital PCR plate, each equating to an individual PCR reaction to detect SARS-CoV-2.
“If you monitor wastewater, you can potentially screen 10,000 people, by analyzing one sample.”
Dr. Warish Ahmed

is a research projects officer specializing in molecular biology and genomics. Suzanne has an MSc in Biochemistry and worked in medical pathology and university research labs before joining CSIRO Land & Water. Prior to turning her attention to COVID-19 wastewater testing, she applied metagenomic techniques to monitoring drinking water quality, and investigated genetic indicators of insecticide resistance.

Scientists in Montpellier, France, have also been turning to dPCR to tackle population-wide screening in wastewater.
When local authorities asked French startup I.A.G.E. to assess the potential impact of the SARS-CoV-2 virus, on a local oyster farm, it did not come as a surprise, recalls co-founder and head of business development Oliver Couillerot. Specializing in environmental biological analysis and dPCR, the company had collaborated in the past to measure the impact of human activities on the Thau lagoon, home to a thriving shellfish industry and 10% of France’s annual oyster production. Oysters are known for their ability to clean the waters they call home because as they feed, they trap bacteria and other harmful contaminants. The impact of wastewater overflow had long been a concern of oyster farmers in the area, and now they faced a new threat – SARS-CoV-2.
Scientists at I.A.G.E. had already established a robust approach to quantify the SARS-CoV-2 virus in wastewater, incorporating QIAGEN’s QIAcuity instrument. “Our diagnostic test relies on digital PCR,” Couillerot says, “because it’s a very sensitive and reproducible tool to measure the amount of DNA and RNA molecules in a sample.”
What they found in the samples taken near the lagoon was more than a big surprise: their test revealed not only SARS-CoV-2 but the UK variant of the virus – the first evidence of this variant in France.
The dPCR test has since shown its value in correlating viral loads in sewage with diagnostic testing and tracing variants of SARS-CoV-2. “It allowed us to perform global and massive monitoring of the infection levels in a population within a city, and even smaller communities, such as residential settings for elderly people,” says Couillerot. The company plans to make the tool available at a reasonable cost to researchers for whom sophisticated assays might otherwise be out of reach. “And to do that, we rely on the QIAcuity, because of its rapidity in processing samples, reliability of results obtained, simplicity of use and affordable price.”

- Launched in September 2020
- Orders for the QIAcuity series of digital PCR platforms reached over 200 at the end of 2020.
- ~$300 million digital PCR market and ~20% CAGR